What Is Hypertension?
Hypertension, or high blood pressure, is a very common condition affecting almost half (45%) of the U.S. population, or 108 million adults. Hypertension occurs when the pressure of the blood flowing through the arterial blood vessels is consistently high. This can cause many serious health consequences, including a higher risk of heart attack, stroke, heart failure, headaches, nosebleeds, and kidney problems.
Hypertension is diagnosed when there are at least three separate elevated blood pressure readings (as defined below), on different days and at different times of the day.
High blood pressure accounts for about 32 million doctor office visits and about 1 million emergency room visits per year.
Less than half of patients with hypertension have their blood pressure adequately controlled.
The first step in controlling your blood pressure is to become educated about this condition, how to monitor it, and how to correct it.
Understanding Your Blood Pressure Numbers
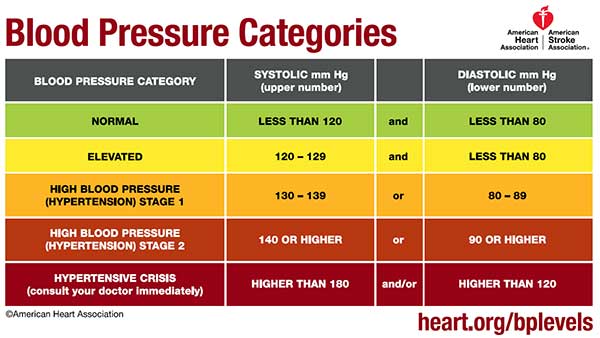
Your blood pressure measurement is reported as two numbers separated by a slash. The top number, or systolic, refers to the pressure in the blood vessels when the heart is expelling blood to the body. The bottom number, or diastolic, refers to the pressure in the blood vessels while the heart is relaxed, or in between heartbeats.
The blood pressure is measured in units of millimeters of mercury, or mmHg. The blood pressure is typically recorded by an electronic or battery-operated machine that a patient can use at home. It can also be measured manually which requires the use of a stethoscope, with a device called a sphygmomanometer; this is usually performed in a doctor’s office.
Normal blood pressure is now considered to be less than 120/80 mmHg. Blood pressure readings that are consistently elevated above this are considered to be hypertension.
According to the American Heart Association, systolic blood pressure of 130 mmHg or above, or diastolic blood pressure of 80 mmHg or above is considered stage 1 hypertension. More information is available at www.heart.org.
Risk Factors for Hypertension
Some factors make it more likely for you to develop high blood pressure.
1) Dietary intake
A number of dietary items can raise blood pressure. A big dietary culprit in causing high blood pressure is high salt or sodium intake.
Adding extra salt to your food, or ingesting too many sodium-rich foods can result in high blood pressure readings. Many people are unaware of how high the salt content can be in the foods they regularly ingest.
High salt food items include many canned soups, frozen dinners, canned vegetables, various sauces, and salad dressings, cheeses, bread, and tomato juices. Restaurant foods tend to be particularly high in salt.
The recommended daily sodium intake should be less than 2,300 milligrams; some experts recommend the daily value should not exceed 1,500 milligrams. The extra salt that is ingested causes fluid and water retention, which puts more pressure on the blood vessels and results in elevated blood pressure.
Caffeine and alcohol use can also raise blood pressure. Caffeine should be limited to the equivalent of two cups of coffee per day. Caffeine can also be found in colas, teas, chocolate, and energy drinks. Caffeine is a stimulant that can increase the systolic and diastolic blood pressures by about 10 mmHg from your normal baseline. The usual onset of caffeine stimulation occurs between 30 to 120 minutes after drinking it.
Men should not have more than two alcoholic drinks per day, and women should not have more than one alcoholic drink per day. An alcoholic drink is defined as 12 ounces of beer, 5 ounces of wine, or 1.5 ounces of 80-proof distilled spirits.
Tobacco use can increase blood pressure. The nicotine causes increased stress and pressure on the heart that leads to elevation of blood pressure.
Decongestants, steroids, and anti-inflammatories can raise blood pressure. Decongestants cause narrowing of the blood vessels which increases blood pressure.
Steroids and anti-inflammatories (such as ibuprofen) can increase blood pressure by causing an increase in fluid retention.
Dietary supplements and herbal remedies can raise blood pressure. If you have high blood pressure, you should check with your physician before starting to take any over-the-counter supplements or herbs.
Ingestion of black licorice can raise blood pressure. Licorice contains the chemical called glycyrrhizin acid, which causes low potassium and raises blood pressure. Usually, a person would need to be eating at least one ounce per day of the black licorice for one to two weeks to see the rise in blood pressure. Nonetheless, one should ingest licorice cautiously and sparingly.
2)Age
Blood vessels stiffen as we age and can lead to elevated blood pressure readings.
3)Family History of Blood Pressure
Family history of high blood pressure – genetic factors can make it more likely for you to develop high blood pressure
4)Diabetes
Elevated blood sugar can affect all the blood vessels of the body and can contribute to high blood pressure. Diabetics are twice as likely to develop hypertension than those without diabetes.
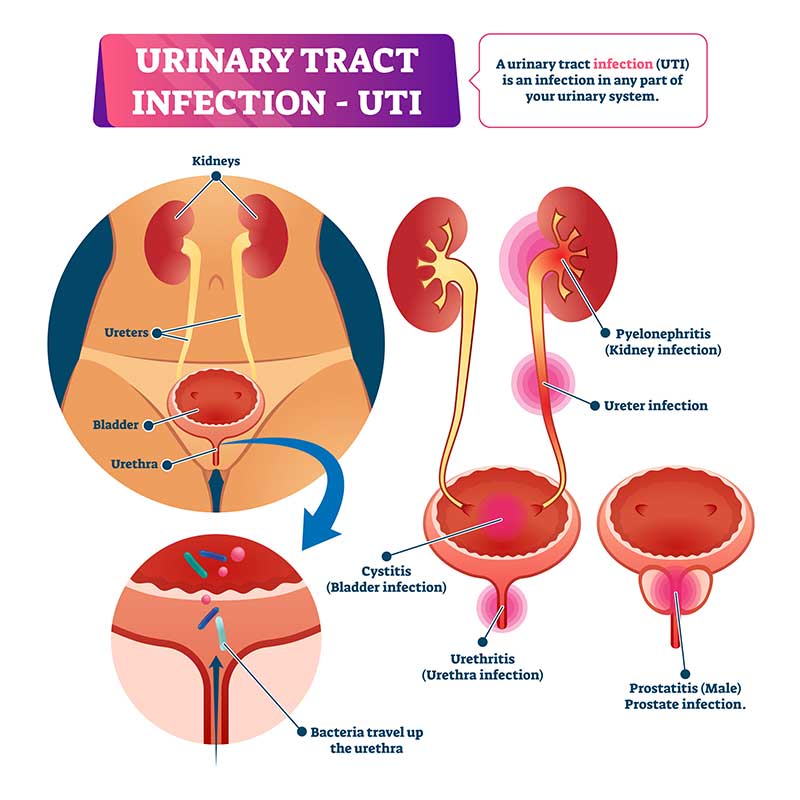
5)Kidney or thyroid problems
Kidney and thyroid issues can affect the hormones in the blood and make it more likely for you to develop high blood pressure. Treating the underlying kidney or thyroid problem with medication can sometimes help the blood pressure to be adequately controlled.
6)Obstructive Sleep Apnea
Obstructive sleep apnea, in which a patient stops breathing multiple times per night, can promote high blood pressure and heart rhythm problems as well. Sleep apnea can be diagnosed by tests ordered by your physician, including an overnight sleep study, or polysomnography test.
If you have sleep apnea, there are ways to help control it, which in turn help bring the blood pressure under better control.
Signs and symptoms of high blood pressure

Sometimes a person may have no symptoms of high blood pressure at all. For this reason, hypertension is sometimes called “the silent killer,” because high blood pressure can be life-threatening, regardless of how you are feeling.
Often, however, a person may note headache, flushing or warm sensation, nosebleeds, or dizziness. These can be signs that the blood pressure is elevated. You should check your blood pressure at home or have it checked at your doctor’s office. If in fact your blood pressure is high, especially on more than one occasion, it may warrant the use of blood pressure-lowering medication on a daily basis.
When is high blood pressure an emergency?
High blood pressure can become an emergency depending on your symptoms and the length of time that the blood pressure remains elevated.
Symptoms can occur with even mildly elevated blood pressure, but if your blood pressure remains above 180/120 mmHg, this is called a hypertensive crisis and you should seek immediate medical attention. Serious consequences, such as heart attack and stroke can occur if the blood pressure is not lowered quickly and carefully.
What to do if you suspect a hypertensive crisis
If you suspect a hypertensive crisis, assess yourself for concerning symptoms such as chest pain, shortness of breath, headache, blurred vision, slurred speech, or difficulty moving the arms or legs.
If any of these symptoms occur, immediate evaluation at the closest urgent care center is necessary. You should not drive yourself to the hospital; ideally, you should call an ambulance, or have someone drive you there. You will be given medication, possibly intravenously, to lower your blood pressure and reverse your symptoms.
You will need to be monitored closely. Blood work will be done to look for potential damage to the heart, kidney, and other organs, and to help determine the underlying cause of the blood pressure elevation. Your condition can change from stable to unstable quickly, so it is important to be fully evaluated and tested in a medical setting.
How to manage hypertension
The first step in managing high blood pressure is lifestyle modification. Eating a healthy diet and increasing exercise can go a long way in improving and sometimes curing high blood pressure.
Lifestyle changes include following a low sodium diet, with sodium or salt intake at least below 2,300 milligrams per day, ideally between 1,500 to 2,300 milligrams per day.
Limiting alcohol to one alcoholic drink per day for women and two alcoholic drinks per day for men also helps control blood pressure. Alcohol can stimulate the heart, and in excessive amounts, can weaken or damage it.
Limiting caffeine and tobacco intake, and ideally, abstaining completely from these products helps control the blood pressure as well. Caffeine stimulates the heart by raising blood pressure and heart rate. The nicotine in the tobacco constricts the blood vessels, thereby raising the blood pressure.
More information on maintaining a heart-healthy lifestyle is available on www.cdc.gov and www.nhlbi.nih.gov.
If your blood pressure remains elevated despite lifestyle modification, your physician may prescribe blood pressure pills, also called anti-hypertensive medication.
There are many different classes of these pills available; each has benefits and potential side effects. Your physician will work with you to find the proper medication and dosage that minimizes side effects. Many of these drugs are available in generic form rather than brand name, making them more affordable.
Common High Blood Pressure Medications
Some of the commonly used anti-hypertensive medications are described below. You can find out more information on www.mayoclinic.org.
Diuretics, also called “water pills” – this group acts by causing the kidneys to release extra sodium and water from the body by urinating it out, thereby reducing the blood pressure. Commonly used examples include hydrochlorothiazide and furosemide. Side effects can include low potassium levels, kidney problems, and dehydration.
If you are taking a diuretic, you may also be prescribed a potassium supplement, since your potassium levels can be reduced in addition to the sodium and water levels in your body. Usually, routine blood work should be performed while you are taking a diuretic, to ensure that your potassium and kidney function remains normal.
Typically, it is recommended that a diuretic is a first-line medication to use for someone diagnosed with high blood pressure. If you already have significant kidney problems, this class of medications may not be ideal for you.
Beta blockers – this group of medications acts by slowing the heart rate down and relaxing the force of the heartbeats, which lowers the blood pressure. Commonly used medications in this group include atenolol, metoprolol, and propanolol. Common potential side effects include fatigue and low heart rate, or pulse.
Calcium channel blockers – this group of medicines prevents calcium from entering the heart cells.
Without calcium, the heart does not contract as forcefully and the blood vessels are more relaxed, thus blood pressure is lowered. Common examples of calcium channel blockers include amlodipine, diltiazem, and verapamil. Side effects can include constipation and leg swelling.
Angiotensin converting enzyme inhibitors, also called ACE inhibitors – these medications work by blocking the production of angiotensin II, which normally produces a hormone that raises the blood pressure. In this way, the blood pressure is lowered.
Commonly used ACE inhibitors include lisinopril, enalapril, and benazepril. Potential side effects can include cough and high potassium levels. The kidney function should also be monitored while taking this medication. Additionally, this medication should be avoided during pregnancy.
Angiotensin II receptor blockers, or ARBs – this group of medication is closely related to ACE inhibitors as mentioned above. The ARBs block the action of angiotensin, which is a chemical that narrows the blood vessels.
When angiotensin II is blocked, the blood vessels are relaxed and the blood pressure is lowered. Similar to the ACE inhibitors, these medications can cause elevated potassium levels and can affect kidney function; these values should be closely monitored with routine lab work. Commonly used ARBs include losartan, olmesartan, and valsartan.
Monitoring your blood pressure

If you have high blood pressure, it is a good idea to invest in a home blood pressure monitor so that you can track your blood pressure on a regular basis. These monitors can be purchased at your local drug store. These monitors are designed to be easy to use. They are typically automated; with the push of a button, the cuff inflates and then digitally displays your blood pressure as measured in mmHg, and heart rate (pulse) in beats per minute.
The blood pressure machine has an inflatable cuff that is placed on the upper arm, or on the wrist. The machine type that uses the upper arm is usually the most accurate. Make sure that the cuff is not too loose or too tight on your arm, otherwise, this can make the blood pressure reading inaccurate.
You can track your blood pressure first thing in the morning, before you take any pills, to get an idea of your actual baseline blood pressure reading. You can check your blood pressure an hour or two after you take your morning blood pressure medicine to see if the medication is starting to work to lower your blood pressure. You can check your blood pressure in the evening, to see how the stresses of the day have affected your readings.
As mentioned above, your blood pressure can be significantly elevated without any symptoms. Even if you take blood pressure-lowering medications, it does not guarantee that your blood pressure will stay under good control.
Other factors can raise your blood pressure even when you are taking these medications, including low back pain, physical or emotional stress, or excess salt or caffeine intake.
Blood pressure medication dosages may need to be adjusted to help maintain adequate control throughout the day. Some blood pressure medication may need to be taken up to four times per day for best results.
When preparing to check your blood pressure, you should first sit quietly for a few minutes and rest. If you check your blood pressure right after rushing in from exercising or after a stressful incident, it will likely be elevated and not reflect your actual baseline.
You should have your feet resting on the floor and not have your legs crossed.
Try to avoid checking your blood pressure soon after having your morning coffee., as this can also raise your blood pressure.
The arm with the blood pressure cuff should be placed on with your arm outstretched and palm upright, with your upper arm aligned near your heart level for most accurate results; your arm should not be dangling down at your side while the monitor is calculating your blood pressure.
From time to time, you should check your blood pressure in each arm, and make sure the readings are the same or close to the same; if you notice a large difference in the blood pressure readings between the two arms (greater than 10 mmmHg difference in either the systolic or diastolic number) notify your doctor, as this may warrant further testing for a possible blockage in the arteries of the arm.
When preparing for your doctor’s visit, it is a good idea to bring a written blood pressure log listing the date and your blood pressure readings, so your physician can review the trend and determine if any medication adjustments need to be made.
If you have been noticing that your blood pressure readings are fluctuating a lot, or if your blood pressure is not under good control despite taking your medication as prescribed, you should bring the actual blood pressure cuff to the doctor’s visit, to compare your cuff reading against the office’s blood pressure device, which is calibrated and routinely checked for accuracy.
Sometimes, with the usual routine and repeated use, the home blood pressure cuffs can lose their accuracy. Changing the battery may help to recalibrate the machine and restore the accuracy of measurement; other times, the machine may need to be replaced if it is not measuring similarly to the doctor’s office blood pressure reading.
Compliance with blood pressure medication
For millions of people, taking one or more daily blood pressure medications is a way of life. It is vital for the proper blood pressure pill to be prescribed so that you can easily tolerate it. Considerations in choosing the best medication include cost, potential side effects, medication interactions, and frequency of dosing.
When you are prescribed a new blood pressure medicine, you should closely monitor and record your blood pressure morning, noon, and night, to get an idea of the trend of your blood pressure and how you are reacting to the medication.
If your blood pressure is still elevated despite taking your medication as prescribed, the dosing or frequency of dosing may need to be adjusted. In some cases, a second, or third blood pressure medication may need to be added to best control the blood pressure.
See also: 6 Ways to Reduce Your Risk of Colon Cancer.
You should also watch out for potential side effects from your medications. These can include headache, dizziness or lightheadedness, leg swelling, cough, or fatigue, among many others. Your doctor can work with you to minimize these side effects; sometimes you may have to be switched to a different blood pressure medication that you can better tolerate.
If your blood pressure is still not under good control despite taking your medication as prescribed, your doctor may order more involved testing to look for secondary causes of high blood pressure. These can include underlying kidney or hormonal problems that need to be addressed separately.
In many cases, if you lose weight, your blood pressure will improve. You may be able to reduce the dose of your blood pressure medication, or even stop it completely; if you continue your current dose, you may notice that your blood pressure is too low and that you are getting dizzy. This should be discussed with your doctor, and you should not change or stop your medications on your own.
The information provided in this article is for educational purposes only. It is not intended to be used to diagnose or treat your specific medical condition. Only a medical provider who examines you and is aware of your medical issues should prescribe medication for you.
if your blood pressure is elevated and you are having symptoms like headache, weakness, dizziness, pain, etc. — you should go to your nearest emergency room or urgent care center, enTrust Immediate Care being a good choice. if you are unable to go safely to an urgent care center, you -should call 911.
—————————————————————————-
 Dr. Kanti Bansal, MD is a founding member of enTrust Immediate Care and an Emergency Medicine Physician in Houston, TX. He has over 20 years of experience in the emergency medical field. Before becoming an attending physician, he served as Chief Resident of his emergency medicine residency at Metropolitan Hospital Center in Manhattan, New York. He holds a Bachelor of Science degree in Biology and a minor in Computer Science from Brandeis University in Massachusetts. Dr. Bansal worked as an emergency room physician for several years at many hospitals in the Greater Houston Metro area, including Memorial Hermann Southwest, Memorial Hermann Southeast, Memorial Hermann Memorial City, St. Catherine’s Hospital in Katy, Texas, as well as St. Mary’s Hospital in Beaumont, Texas.
Dr. Kanti Bansal, MD is a founding member of enTrust Immediate Care and an Emergency Medicine Physician in Houston, TX. He has over 20 years of experience in the emergency medical field. Before becoming an attending physician, he served as Chief Resident of his emergency medicine residency at Metropolitan Hospital Center in Manhattan, New York. He holds a Bachelor of Science degree in Biology and a minor in Computer Science from Brandeis University in Massachusetts. Dr. Bansal worked as an emergency room physician for several years at many hospitals in the Greater Houston Metro area, including Memorial Hermann Southwest, Memorial Hermann Southeast, Memorial Hermann Memorial City, St. Catherine’s Hospital in Katy, Texas, as well as St. Mary’s Hospital in Beaumont, Texas.